For most people a painful crisis is the usual problem in sickle cell. Crises occur again and again and are the most frequent reason for admission to hospital. The underlying reason for a painful crisis is blockage of small blood vessels by sickled red cells which, by restricting blood flow, starves the tissues of oxygen and results in the death of tissues and cells leading to pain. The usual tissue affected is the bone marrow, which is found inside the bones and which is why, in 99% of cases, the pain of a crisis is felt coming from the bones. But vaso-occlusion, as the process of blood vessel blockage is called, can affect any tissues and organs in the body and I thought it would be useful to review some of these other effects of sickling and associated complications. I will start with the lungs and in future blogs discuss the kidneys and liver. Any other ideas gratefully received.
What do the lungs do?
Everyone knows that the lungs are for breathing. Each time we take a breath air flows into the deepest parts of the lungs where only a thin membrane separates the air from the blood. Oxygen passes across the membrane, enters the red blood cells and binds to haemoglobin, both normal and sickle haemoglobin. The red cells then carry the oxygen all around the body, delivering it to cells and tissues where it provides the energy which powers all the processes keeping us alive.
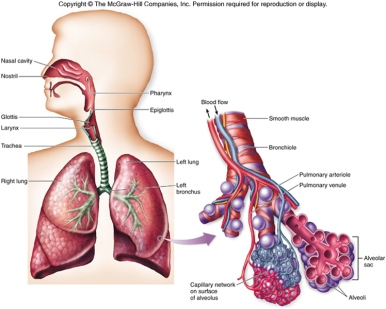
Air is drawn into the lungs by the action of muscles – the diaphragm, a muscle sheet which separates the chest from the stomach, and the intercostal muscles between the ribs on each side of the chest. The air flows into little, thin walled sacs or alveoli where it is in very close proximity to the blood and where oxygen exchange takes place.
How do we assess how well the lungs are working?
Because of the importance of the lungs your doctor they will make an assessment of how your lungs are working nearly every time you see them. Important symptoms to tell your doctor about include being short of breath, any pain in the chest when breathing, any wheezing or cough and any blood in your sputum or phlegm. The simple stethoscope is a useful way of listening to the noise the air makes as it flows into and out of the lungs, which can give a lot of information about how the lungs are working. In addition, almost all of you will have had a chest x-ray on many occasions, which allows your doctor to look at the lungs and see if they are as full of air as they should be.
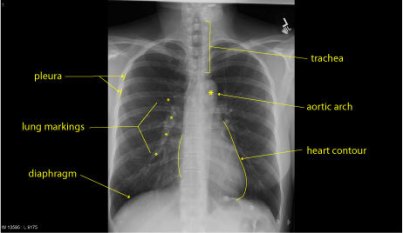
This is normal chest x-ray. The pleura are the membranes which cover the surface of the lungs and help them to move freely within the chest. The trachea or windpipe delivers air to the lungs. The lungs themselves, if they are full of air are black, the markings on them are the blood vessels and small airways, along which blood and air travel to the alveoli. The heart is the white shadow in the centre of the chest. Bones also appear white and you can see the ribs curving around the chest.
Other tests which your doctor may request include measuring the amount of oxygen in the blood stream; the oxygen level, or O2 saturation, indicates how efficiently the lungs are working.

Oxygen saturation is normally measured by a probe which fits over a finger. It will not work properly if you are wearing nail varnish or have false nails. The usual value is close to 100%; values less than 96% may be an indicator that the lungs are not delivering oxygen to the blood effectively.
Less often your doctor may ask you to do “spirometry” to measure how quickly you can expel air from the lungs, this is called “the peak expiratory flow rate” or PEFR and tells your doctor if the airways that the air flows through are too narrow. The PEFR can be measured at the bedside but for more detailed information about how the lungs are working you may have to go to the Lung Function Laboratory for a full set of lung function tests.
What special problems are the lungs prone to in sickle cell disease?
Lack of oxygen is one of the factors which promotes sickling, and that is why the lungs and oxygen delivery are of particular importance in sickle cell disease. Any problem involving the lungs is likely to be complicated by a painful crisis as well. It is useful to think of these lung problems in two groups; acute problems which are short term and generally more easily managed if they are detected early and chronic, or long term problems, which are often more difficult to sort out and treat.
Acute problems
1. Infection – chest infections or pneumonia are common and usually present with a fever, cough and pain in the chest. Almost inevitably the infection will also provoke a painful crisis. Parts of the lung, usually on one side only, fill up with infected material, air cannot penetrate and as a result the lungs may be unable to transfer sufficient oxygen into the blood and the oxygen saturation in the blood will fall.

The circled, white area is infection or pneumonia in the right lung. Very little air is able to penetrate the infected area so that part of the lungs cannot contribute to oxygen exchange.
Either bacteria or viruses can cause a chest infection and it can sometimes be very difficult to distinguish between them. The normal treatment involves giving additional oxygen and antibiotics, although only the bacterial pneumonias will respond to antibiotics. The earlier treatment with antibiotics starts the quicker the response.
What can you do? People with sickle cell are particularly susceptible to chest infections. It is therefore very important to take preventative penicillin tablets every day as protection and to make sure you are up to date with all your vaccinations, including having the “flu” vaccine every year to protect against influenza.
2. Acute chest syndrome this is a serious complication of sickle cell, particularly common in children and young people. The way it presents can be very similar to pneumonia, but it usually affects both lungs rather than just one. Pain in the wall of the chest is frequent and often the oxygen saturation falls very low. There are many factors which can trigger the acute chest syndrome but probably the commonest is sickle bone pain affecting the ribs, breastbone and the back of the chest. Severe pain makes it very difficult to breathe deeply and as a result the deepest parts of the lungs are starved of air and oxygen and the red cells passing through these parts will sickle, blocking blood flow and causing the death of lung tissue downstream. This results in inflammation and the rapid build up of fluid in the lungs.
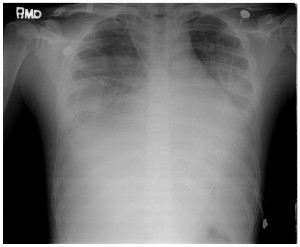
This chest x-ray shows almost complete “white out” of both lungs due to the collection of inflammatory fluid in the alveoli. The fluid further restricts oxygen uptake, promotes more sickling and leads to a vicious cycle of deterioration.
Treatment needs to be quick and aggressive to get on top of this process. Extra oxygen and fluids help but the key intervention is an exchange blood transfusion which, by removing the sickle red cells, stops the process in it’s tracks and allows gradual recovery.
What can you do? If you get rib pain you will be given an incentive spirometer. This is a device to encourage you to take a deep breath and make sure the air gets right down into all parts of the lungs stopping the acute chest syndrome from taking hold. If you use it properly it will make the pain in your ribs worse but it is a very effective, simple intervention which will prevent the acute chest syndrome.

Use the IS every hour. Blow all the air out of your lungs then, with the mouthpiece in place, slowly suck in as much air as you can. Getting the marker up to 2500-3000 is a good effort.
When you go home take your incentive spirometer with you and carry on using it regularly. It’s good exercise for the lungs. Never ignore or underestimate sickle pain in the ribs.
3. Blood clots these usually start in the veins of the legs where they are known as a deep vein thrombosis or DVT. They may cause no symptoms or may cause the calf to swell and become painful. Pieces of the blood clot may break off and travel through the circulation lodging in the blood vessels of the lungs, this is called a pulmonary embolism or PE and can be very serious. Hospitalised patients with sickle cell are particularly prone to DVT’s and PE’s; they are ill in bed, often immobile because of pain and they may have areas of inflammation in their legs due to a painful crisis. All of these factors increase the risk of a blood clot forming. Problems with blood clots are usually treated with drugs, such as warfarin and heparin, which slow down the clotting of the blood, but prevention is much the best option.
What can you do? When they are admitted to hospital most patients with sickle cell will be prescribed a daily injection of low molecular weight heparin (LMWH) which will stop the blood clots forming in the legs in the first place. You can also help by trying to stay active, getting up and walking around the ward if possible and even when lying in bed keeping the muscles in the legs working and the blood flowing by doing regular leg exercises every hour or so.
Chronic problems
1. Sleep disordered breathing affects many people. Breathing may be noisy at night with snoring, which is due to intermittent obstruction to the movement of air through the large airways, or the breathing rhythm may be disrupted with short periods when breathing stops completely. During these episodes the oxygen level in the blood may fall low enough to provoke an episode of sickling, typically causing the person to wake up in the early hours of the morning with a painful crisis. If you think this applies to you talk to your doctor who can arrange for your oxygen levels to be monitored at home whilst you are asleep. If the oxygen saturation is low at night and correlates with you getting a crisis then one solution is to have additional oxygen at night when you are asleep to prevent this.
2. Chronic sickle cell lung disease is a condition which is thought to follow recurrent attacks of the acute chest syndrome. The repeated episodes of inflammation cause fibrous or scar tissue to be laid down in the lungs making them very stiff and inflexible so that they cannot expand properly. The restricted movement of the lungs means that not enough air moves into the lungs with each breath and the amount of oxygen taken up is severely reduced leading to chronically low oxygen levels in the blood. The condition can be diagnosed by having a full set of lung function tests which show reduced lung volumes and limited air movement. Once established, there is little evidence unfortunately that the two long term treatments in sickle cell, hydroxycarbamide and regular blood transfusion, have any positive impact on the condition.
What can you do? Prevention is better than cure. Avoid the acute chest syndrome by regular use of the incentive spirometer whenever you have chest pain. If despite this you continue to have attacks you should take hydroxycarbamide or participate in a programme of regular blood transfusions both of which are very effective at preventing the acute chest syndrome and so avoiding long term lung problems.
3. Pulmonary hypertension is a rare condition and has only recently been recognised in sickle cell patients. It is difficult to diagnose and it is possible that it is often overlooked. It means that the pressure within the blood vessels of the lungs is too high. No one knows why some patients develop this. As a result of the high pressures the heart has great difficulty pumping enough blood through the lungs and oxygen levels in the blood can fall very low. Affected patients complain of extreme tiredness, lack of energy and limited exercise tolerance and they often have a dry cough and a rapid rate of breathing. It is difficult to measure the pressure in the blood vessels of the lungs but it can be estimated indirectly by an echocardiogram, which is a scan of the heart.

An echocardiogram being undertaken. The transducer is moved across the wall of the patient’s chest and the computer converts the sound wave echoes into a visual display which appears on the screen.
Confirmation of the high pressures requires passing a probe into a large vein in the neck or leg and threading this towards the heart until it lies in one of the large blood vessels going to the lungs. Treatment is difficult but the best approach appears to be intensive blood transfusion therapy with regular, automated exchange blood transfusions to keep the level of sickle red cells as low as possible at all times. This both reduces sickling and haemolysis, or the rate at which red cells are broken down. A rapid rate of haemolysis destroys a chemical called nitric oxide which is a natural dilator of blood vessels and would normally help to keep the blood vessels of the lungs wide open and the pressures low.
